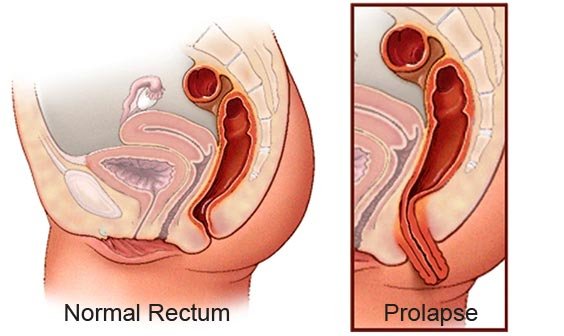
Symptoms of Rectal Prolapse
Bleeding and/or tissue that protrudes from the rectum are common symptoms of both piles (haemorrhoids) and rectal prolapse, but there is a major difference. Rectal prolapse involves an entire segment of the bowel located higher up within the body. Hemorrhoids only involve the inner layer of the bowel near the anal opening. Rectal prolapse can lead to fecal incontinence (not being able to fully control gas or bowel movements)..
Major Causes
While a number of factors are thought to be linked to rectal prolapse, there is no clear cut “cause.” An estimated 30% to 67% of patients have chronic constipation (infrequent stools or severe straining) and an additional 15% have diarrhoea. In the past, this condition was assumed to be linked to giving birth multiple times by vaginal delivery. However, as many as 35% of patients with rectal prolapse never gave birth and it can occur in men.
Diagnosis of Rectal Prolapse
During the first visit, your colon and rectal surgeon will perform a thorough medical history and anorectal exam. In some cases, a rectal prolapse may be "hidden" or internal, making diagnosis more difficult. You may be asked to sit on a toilet at your physician’s office and strain as if having a bowel movement.
Other tests used for diagnosis include:
Videodefecogram: X-rays are taken while you are having a bowel movement to test muscle movement.
Anorectal Manometry: Evaluates muscle functions and reflexes of the pelvis, rectum and anus used during bowel movements.
Treatment for Rectal Prolapse available at Santhosh Hospital
There are several methods used to surgically repair rectal prolapse depending on age of the patient, physical condition, extent of prolapse and the results of tests. Options include removing part of the rectum or pulling the rectum back up and anchoring it. Sometimes mesh is used to reinforce the rectum.
Surgical approaches include:
- Laser Surgery
- Abdominal repair through traditional surgery (open approach)
- Laparoscopic surgery
- Robotically assisted surgery
For a large majority of patients, surgery relieves or greatly improves symptoms. Prolapse or some other condition may have weakened the anal sphincter muscles. However, these muscles have the potential to regain strength after the prolapse has been corrected. It may take as long as one year to determine the impact of surgery on bowel function. Chronic constipation and straining after surgical correction should be avoided.
We have effective perineal repair for rectal prolapse.